The Resurgence of Diagnosis-Related Groups in the AI Era

In the healthcare field, Diagnosis-Related Groups (DRGs) have been a fundamental tool since their origin in 1980. However, their large-scale adoption has faced obstacles, despite their effectiveness in classifying patients and optimizing resources. Today, in the era of Artificial Intelligence, DRGs are resurging. In this article, we tell you about their advantages and challenges, as well as their role in transforming healthcare towards value-based health models.
What are DRGs
Have you ever come across ideas that were revolutionary but perhaps the timing of their appearance wasn’t right? I would dare to say that something similar has happened with the adoption of Diagnosis-Related Groups or DRGs, and that today, for various reasons, they are resurging.
Diagnosis-Related Groups are a patient classification system that allows organizing a hospital’s care activity by relating the different types of patients treated with the cost involved in their care.
Let’s imagine that someone needs care for hip replacement surgery. What that patient represents for the health system that treats them and that an insurer or funder would later have to reimburse to the hospital that provided the services can be determined in different ways.
A classic way is to reimburse one by one all the practices performed (for example, in fees, diagnostic imaging, laboratories, among others), for the consumables required by the patient (disposables, medication, prostheses) and also for the use of different hospital areas (operating room hours, inpatient beds, or others). It’s a logical form, widely used currently, and is called “Fee For Service” or “Pay per Practice”. As you can imagine, it tells us nothing about whether the practices have been appropriate. A risk of this practice is the overutilization of procedures, as there are few incentives for efficiency in the use of resources linked to the medical results achieved in the patient.
Another form of payment, based on historical data of Hip Replacement cases, is to create modules or specific packages based on historical usage rates of practices, services, products, and times that these patients have usually consumed, adjusted for risk profile details and specific characteristics that each case may have.
These modules or packages allow for more accurate determination of the average cost of care, as well as its maximums and minimums derived from the particularity of each case, since medicine is not an exact science, and each patient (and diseases) has its variations (episodes). Ultimately, this module and its cost is what is reimbursed to the care provider.
An advantage of modulated payment models is that they allow for standardization of healthcare activity, making it comparable between different hospitals as well as with care norms or standards. This form, where care is modulated and comparison between patients and institutions is allowed, as well as incentivizing efficiency, is what is known as the International DRG Methodology.
Since their adoption, DRGs have proven to be a fundamental tool for cost control in healthcare and for improving the quality of care. Among their most notable advantages are:
- Greater efficiency in hospital bed management.
- Increased transparency and reduced friction in relationships between payers and medical service providers.
- More effective utilization of resources dedicated to medical care.
- Reduction of administrative expenses that do not add value for payers, hospitals, or patients.
Despite their seemingly simple logic and proven effectiveness over time, the question arises as to why DRGs have not been implemented on a large scale worldwide.
Well, there are nuances…
DRGs offer an efficient way to classify patients according to similar medical care patterns (clinical similarity) and similar costs (iso-consumption). This allows for more accurate resource allocation, benchmarking of care quality, and more precise prediction of costs and reimbursements. However, their implementation can face challenges in terms of data standardization, information requirements necessary for their use, and resistance to change from health systems or their decision-makers.
The implementation of algorithms such as those used in Diagnosis-Related Groups (DRGs), along with the necessary change management during the introduction of a new payment method, is not simply a technical process. The policy surrounding the introduction of the system and the expected change in resources will generate both supporters and opponents. Therefore, solid technical capacity is required from buyers, providers, and health ministries or other relevant regulatory agencies to manage the DRG system, as well as the necessary “change management”.
Among the necessary technical components and processes, we highlight the following:
- DRG Algorithms: The development of a national and public classification algorithm is the most complex task from a technical point of view. For this reason, most countries start with an imported DRG grouping algorithm or are inspired by an existing one, adapting it to the country’s context. International experience shows that adaptations to the health information management system, contracting and payment modalities, as well as adjustments to the imported DRG algorithm, require several years.
- Effective Hospital Information System: The quality of basic data is fundamental for the implementation of a DRG system. However, a DRG system can, over time, encourage and continuously improve data collection for this and other health policy purposes. It is necessary to have electronic medical records based on standardized coding systems, as well as cost accounting systems per episode and per DRG.
Deficiencies in data collection or quality should not be an obstacle for a country or organization to implement a DRG model, as these are tools that contribute to universal health coverage objectives. The incentives established by the system must be carefully considered to ensure that integrated care focuses on people, and not solely on economic considerations.
Why Globant and Avedian?
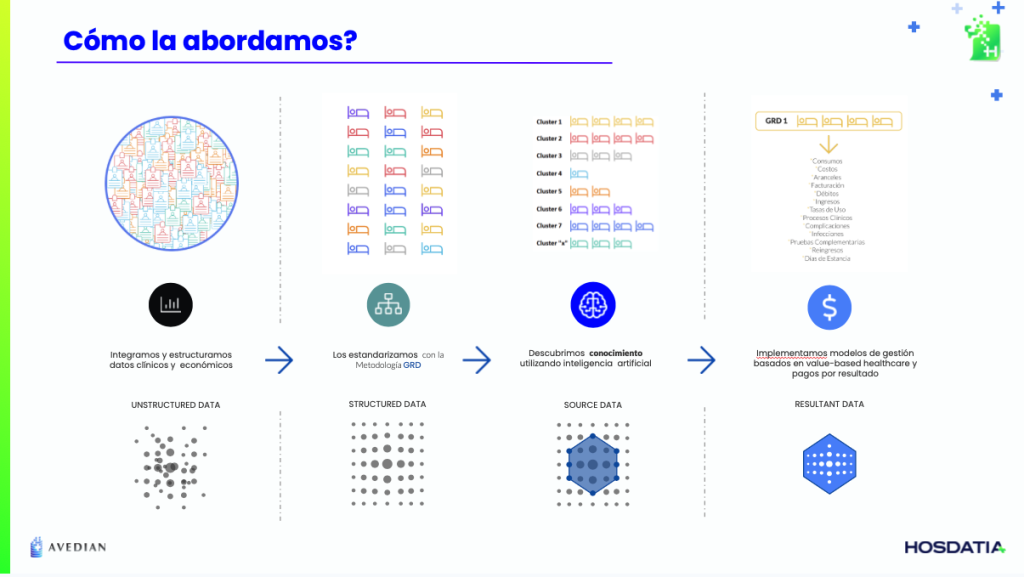
From Globant Healthcare Lifesciences AI Reinvention, we are working together with Avedian to offer advanced digital health solutions that integrate DRGs with AI technologies and data analytics.
Our services include the implementation of end-to-end systems using proprietary DRG algorithms customized to the reality of each country and organization, optimization of hospital workflows, and improvement of healthcare quality through artificial intelligence and the latest technological advances.
With more than 40 implementations in the region, we have the experience, teams, and scale available to transform how healthcare organizations today face challenges such as medical process auditing, increasing costs of innovative pharmaceutical products, and the transformation towards value-based payment models.
One of the differentiators we apply in each project is the capabilities of one of the world’s most admired software and technology companies like Globant, combined with Avedian’s expert knowledge of healthcare systems with their challenges, urgencies, and needs.
The proprietary DRG algorithms, both for hospital and population case-mix, are available from the start in each project, being one of the reasons why our implementation times for projects with a DRG component, whether in analytics or as a payment model, are around two to three months in hospitals and between six and eight months in health insurance.
Authors:
Dr. Guillermo Tabares Martinez – Avedian CEO and Co-Founder
Dr. Lucas Najún Dubos – Globant Healthcare Life Sciences Partner